Welcome to our website
Lichen Sclerosus Association & Network Lichen planus / Vulvodynia
based in Switzerland - active in all of Europe and overseas
Endless itching, burning in the intimate area, frequent fungal infections, white patches, pain during sex, bladder pain similar to bladder infection....
When the genitals itch and burn, it may be caused by lichen sclerosus or vulvodynia or lichen planus. These diseases are common, but not well known, when an accurate diagnosis is so important.
Lichen sclerosus (LS) is four times more common in women than in men. It is assumed that one in 50 women is affected by LS. Men are affected slightly less often. A particular form of LS also occurs in children. In fact, LS does not belong to the category of rare diseases. It is a chronic inflammatory skin disease of the external genital region and is most likely an autoimmune disease that often occurs together with other autoimmune diseases such as Hashimoto's and lichen planus. A familial incidence of up to 50% has been observed. Several causal factors (endogenous or exogenous) are discussed by experts but have not yet been proven. Untreated LS women have an elevated risk for vulval cancer.
 The Lichen Sclerosus Association supports people affected or suspected of being affected by lichen sclerosus (LS), lichen planus or vulvodynia and thei
The Lichen Sclerosus Association supports people affected or suspected of being affected by lichen sclerosus (LS), lichen planus or vulvodynia and thei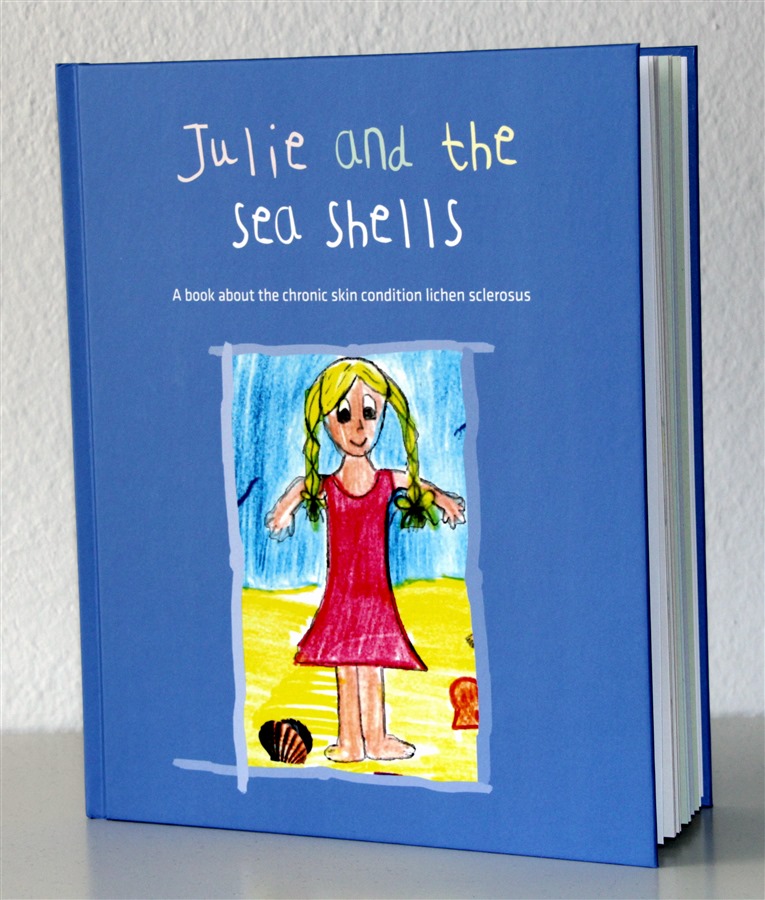 r relatives. It helps sufferrers to live with the disease, to better understand its repercussions, to integrate it into the individual, family and leisure context and to master its consequences. The association is also committed to raising awareness at European level. It has developed various documents: books, booklets, explanatory videos in several languages as well as a short feature movie.
r relatives. It helps sufferrers to live with the disease, to better understand its repercussions, to integrate it into the individual, family and leisure context and to master its consequences. The association is also committed to raising awareness at European level. It has developed various documents: books, booklets, explanatory videos in several languages as well as a short feature movie.
Julie and the seashells - a children's book to help LS girls and their families to better understand and cope with the condition.
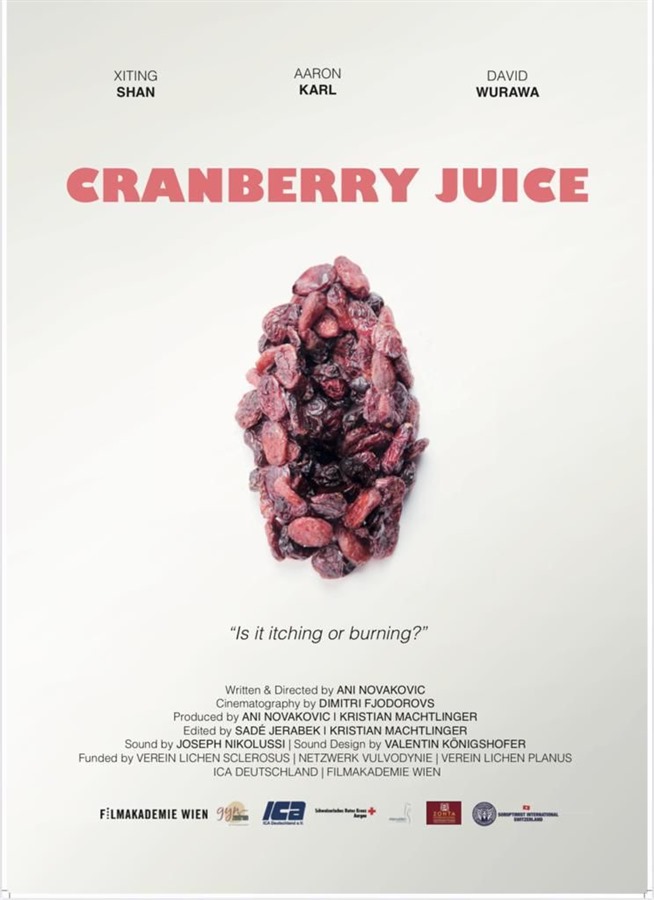
Cranberry Juice - the film describes the long journey to diagnosis for many women.
This website is an information platform and contact network, created by affected people for affected people.
We want to give the disease with the complicated name of "Lichen Sclerosus" (LS) a face, to make it better known to the public and to medical personnel, and to remove the taboo surrounding it. Far too many people suffer for an unnecessarily long time before finally being diagnosed. We are committed to ensuring that affected women, men and children are diagnosed earlier, and treated properly thereafter.
On our website, you will find, free of charge, expert information about the disease and its treatment. This information has been compiled since 2013, and is continuously being updated, in particular the "Information for doctors" tab. Show the documents stored there to your doctor, if you feel there is a possibility that you have the disease.
LS sufferers, or people who think they may have LS, who would like advice, who are looking for a knowledgeable doctor and/or who would like to exchange information with other sufferers, are welcome to contact our board, after having applied for membership. By becoming a member and paying the membership fee, you are supporting our efforts to make LS better known. We guarantee that all members' data is treated confidentially. We ourselves have experienced the taboo surrounding the disease, so data protection is very important to us. If you are interested in becoming a member, please click on the "Become a member" tab. We are also a contact point for people affected by lichen planus and lichen ruber, as well as for women with vulvodynia and associated diseases which sometimes occur in parallel with, or as a result of, LS.
LS is not a death sentence. LS is not curable, but it is treatable. With the right treatment, most sufferers get their symptoms under control and can enjoy an almost painless and happy life again. We would like to give hope to all LS sufferers, and especially to the newly-diagnosed. We see our Association as a life-raft in the ocean of pain, both emotional and physical, for the newly-diagnosed. Between our homepage and the expert information provided, we see ourselves as a refuge for all those who are looking for serious information on the subject.
Our Association was founded in 2013 in Switzerland, and it is now active and present throughout Europe. More than 13'000 members from over 21 countries have already signed up for a membership.
We hope you'll find answers to your questions thanks to this homepage.
We would like to be THE contact-point for you that we would have liked to find ourselves years ago.
At the moment, we are in the process of translating the website from German into English. Thank you for your patience. Please use the free translating machine DeepL (www.deepl.com) or google translate for the moment to help you read the German sections and documents.
With care and absolute discretion, we will personally look after and advise all those who contact us and sign up for membership.
Registered members profit from a protected exchange forum in English.
WELCOME!
"Hope is like a path. In the beginning it does not exist; it forms only if many people go the same way".
(Lu Xin)
Lichen Sclerosus Association - founded in Switzerland, active throughout Europe
Please note that the Board consists of people directly affected by LS, who refrain from introducing themselves by name in the public area of the homepage. We are a non-profit association, and we work on a voluntary basis (see our statutes). Since 1 January 2018, our charitable association has been tax-exempt and is on the list of officially tax-exempt organisations in Switzerland. Contributions and donations to our association are tax-deductible in Switzerland. We are clarifying the situation regarding donations from abroad.
Flyers and Articles:
Association Flyer PDF in English
- 2015: EDF-guideline on Lichen sclerosus, written by Dr. Kirtschig and her co-workers (Download PDF)
- 2017: Leading Opionions Gynaecology & Obstetrics (Translated article) : Lichen sclerosus, under-estimated and under-diagnosed PDF
- 2018: Diagnosis and treatment of vulvar Lichen sclerosus, Update for Dermatologists, Amercian Journal of Clinical Dermatology, Dr. Gayle Fischer
- 2019: On June 13th 2019, our Association was awarded with the Red Cross Award 2019: PDF
- 2020: Article by Susan S. Cooper: Patient education: Lichen sclerosus (Beyond the Basics); Cooper Susan M., et al; uptodate 2020 (PDF)
-
2020: Medscape, Lichen Sclerosus Treatment & Management, Updated: Sep 25, 2020, Author: Lisa K Pappas-Taffer, MD; Chief Editor: William D James, MD (PDF)
- Consultation on urethral constrictions, ICUD on Urethral Structures, SIU/ICUD, L. Stewart, K. McCammon, M. Metro, R. Virasoro (PDF)
- Effect of lichen sclerosis on success of urethroplasty, M. Granieri, A. D. Peterson, R.I. Madden-Fuentes (PDF)
- 2023: EDF-guidline Update on Lichen sclerosus, written by Dr. Kirtschig and her co-workers, including 3 members of our association (PDF)
- 2024: Medscape, Article on Lichen sclerosus: Silent genital health concern often missed (Link www.medscape.com/viewarticle/lichen-sclerosus-silent-genital-health-concern-often-missed-2024a100039j))
- 2024: Lichen sclerosus and me: the male perspective (PDF), by Chris Stanton and Rosalind Simpson
- 2024: A hundred paper cuts over my vulva: a patient's experience of vulva lichen sclerosus (PDF), by Jaclyln Lanthier, Louise Clarke and Rosalind Simpson.
For more articles (in German and English see here)
LINKS:
Videos:
Videos about Lichen Sclerosus and our Swiss Association
- Video (17 minutes), September 2016, Santemedia Medicaltalk, broadcast on regional Swiss channels such as Tele M1, Tele Basel, Tele Bärn, Tele Züri, and Tele Ostschweiz
- Video (7 minutes), 13 February 2017, Lichen Sclerosus - Wissenslücke bei Gynäkologen (gynaecologists' knowledge gaps), Swiss National TV SRF 1 PULS
- Video September 2020 (7 Minutes) , Health Check-UP, broadcast on regional Swiss channels such as TeleM1, Tele Züri, Tele Bärn, Tele
- an many more (as per 2024)
=> see all of these videos and broadcasts on our youtube channel (in German, partly also in French and Italian)
Video on LS in English:
https://youtu.be/nvfzzuMPGm0 / Jill Krapf - Lichen Sclerosus - what is happening on skin level
https://www.youtube.com/watch?v=EyeLlKt-EO8
https://www.youtube.com/watch?v=nLD7BMJHWzA
https://vimeo.com/485988854/13967c9c7e?fbclid=IwAR3Wl9ywhmL2bS4LjVmLCm6C5JVqQjIrNYkHXPq4Mh-AXzSG6SUs4CcMr64
Other Websites and Networks:
Facebook-Groups:
- Ein Leben mit Lichen sclerosus (German)
- Natural Lichen sclerosus solution (English)
- Lichen sclerosis - Lichen sclerosus meeting of the Minds (German and English)
- Lichen Planus Support Group (English)
- Lichen scléreux ou scléroatrophique - Groupe de soutien (French)
- Lichen Sclerosis / Sclerosus: Healing naturally through nourishment (English)
- Lichen Sclerosus in men (English)
In men, whitish coatings and painful skin changes initially appear on the foreskin, and perhaps also on the glans.
In children, mostly girls, there is often a symmetrical reddening of the outer labias. There is sometimes also a whitish film, which is often confused with nappy rash in infancy.
See our book "Julie and the seashells under "book shop" / Book-Flyer PDF
In boys, LS is almost always accompanied by narrowing of the foreskin.
If you suspect, after self-examination, that you have LS, please contact a doctor who is familiar with the disease and have it examined. The doctor can then rule out or confirm the diagnosis and, if confirmed, initiate treatment in accordance with the European Treatment Guidelines (see below).